Mastitis is an inflammation of breast tissue that often leads to an infection and may cause tenderness and pain. Having mastitis can be very frustrating, especially if you are breastfeeding, but there are steps you can take to treat it and relieve some of the symptoms. Read more below to find out what causes mastitis, and how you can prevent or treat it. You can also refer to our complete downloadable breastfeeding guide to learn about mastitis and best practices for successful breastfeeding.
What Is Mastitis?
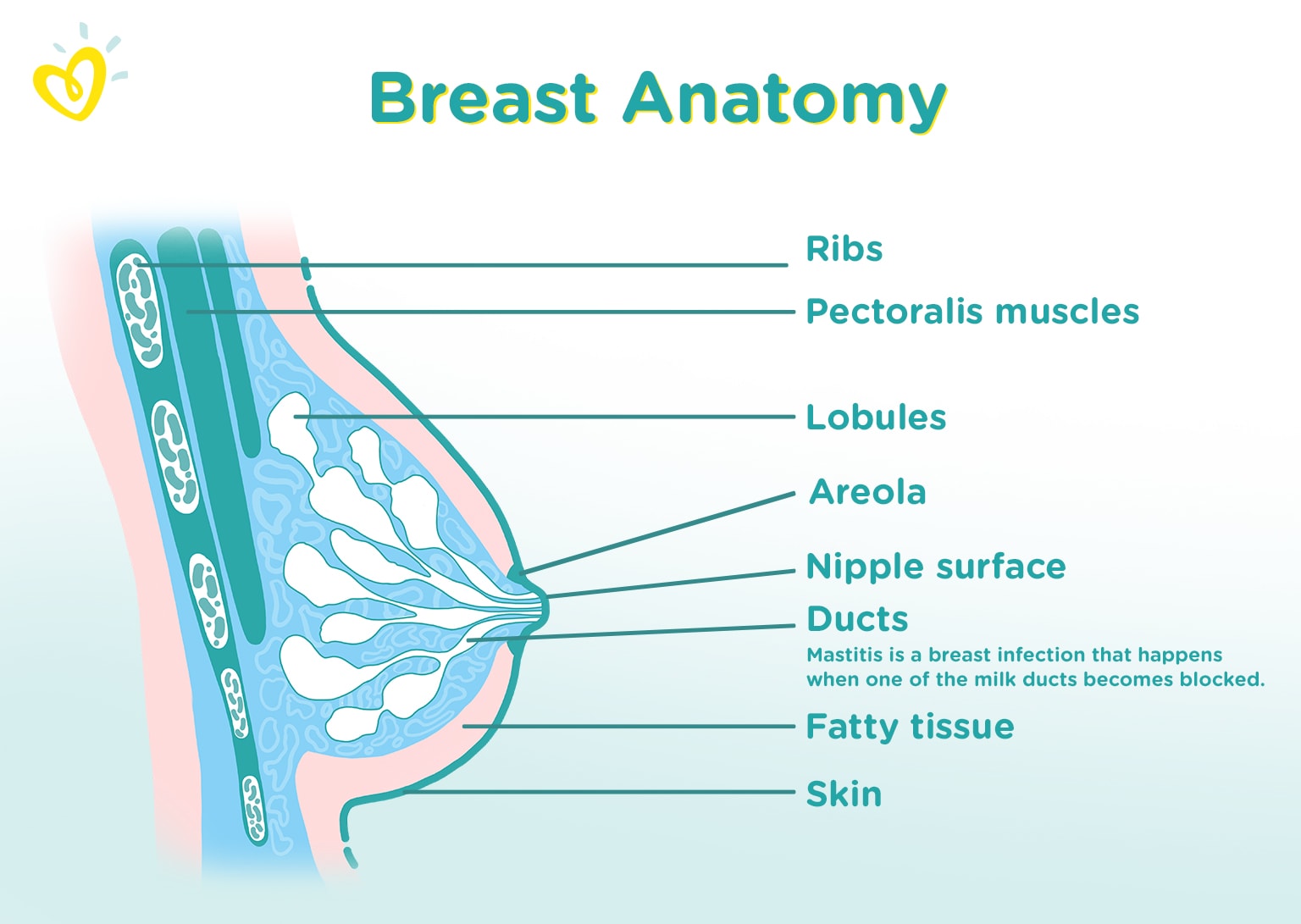
When a buildup of milk causes a milk duct in your breast to get blocked, the breast can become inflamed and mastitis can result. A hard lump can form, and the breast becomes tender and sore. In the case of lactating moms — breastfeeding moms and moms who are pumping breast milk — this condition is specifically called lactation mastitis.
Signs and Symptoms of Mastitis
You may wonder what mastitis feels like compared to the normal tenderness you might feel when you first start breastfeeding. Or, you might wonder what mastitis looks like. Some of the signs and symptoms of mastitis include
- flu-like symptoms such as fever, fatigue, and aches
- a hard, tender lump in one breast
- red patches on the breast
- swelling of the breast
- the breast feeling warm to the touch
- a burning sensation while breastfeeding.
What Causes Mastitis?
These are some of the risk factors that might increase your chance of developing the mastitis infection:
- Incorrect breastfeeding technique. If you don't vary your breastfeeding positions or don't fully empty each breast, for example, the milk can build up and can become trapped in the milk ducts.
- Clogged milk ducts that aren't cleared in time. If a milk duct gets clogged with milk, a hard and tender lump will form. If the clogged duct isn't cleared, an infection can set in.
- A crack or blister on the nipple. A crack in the skin of the nipple or a milk blister can lead to a bacterial infection in the breast. A milk blister is a painful white spot on or near the nipple. It isn't the same as a blister caused by friction from an incorrect latch from your baby while feeding; it's a spot of thickened milk near the opening of the nipple that may block the flow of milk.
- Constraining your breasts. Wearing a bra that is too tight or putting pressure on your breast (for example, from the strap of a heavy bag) can restrict the flow of milk.
- A weakened immune system. Being overly stressed or fatigued, or having poor nutrition can suppress your immune system and make you more susceptible to the mastitis infection.
- Previous bouts of mastitis.
- Smoking.
When Should I See a Doctor?
Early treatment of mastitis is important. Speak with your healthcare provider or lactation consultant if the earliest signs of mastitis don't clear up promptly. A spike in fever, pus or blood in your milk, and red streaks from your nipple to your underarm are signs that the mastitis infection has worsened. If left untreated, symptoms can worsen and an abscess can form.
Treatment for Mastitis
If you have mastitis, your healthcare provider will usually prescribe antibiotics that are safe for your baby, too. You should begin to notice improvement within a day or two, but it’s important to take the full course of antibiotics, even if the symptoms clear. Breastfeeding won’t hurt your baby — the milk itself isn't affected — and nursing will actually help clear the infection. Your healthcare provider might also suggest taking a painkiller to help ease the discomfort. If you have recurring bouts of mastitis, or the infection doesn’t seem to go away, contact your provider again.
In addition to the treatment your provider recommends, you might try some of these self-care methods to relieve some of the symptoms of mastitis:
- Drink plenty of fluids and get ample rest.
- Fully drain the milk from each breast at each feeding. If nursing is too painful, try hand-expressing or using a breast pump instead.
- Don’t reduce feeding times, as this can cause your milk supply to drop, prolonging recovery. Read more about increasing your breast milk supply.
- Keep to a regular feeding schedule as much as possible. If something should interrupt this schedule (like your return to work , for example) try to express milk around the same time you’d normally be breastfeeding your baby.
- Apply wet or dry heat to the affected breast just before breastfeeding or expressing. A warm compress can work well, or you could take a warm shower. You can also fill a clean sink or basin with warm water and lean over it to soak the affected breast.
- Massage your breasts gently while they’re warm and then try breastfeeding or expressing milk, or gently massage the affected area on your breast while breastfeeding.
- Go braless and wear loose-fitting tops.
- Applying cold cabbage leaves is sometimes recommended as a home remedy for breast engorgement, although there is limited research that supports its usefulness. Hot and cold compresses are more effective for reducing the discomfort of engorgement that is sometimes a symptom of mastitis.
Can You Breastfeed if You Have Mastitis?
Mastitis does not cause your milk to become infected, and your baby won’t be harmed by nursing. Although breastfeeding with mastitis may be uncomfortable at first, continuing to breastfeed will not only speed up recovery and help keep the mastitis from worsening, it will also help keep your baby’s immune system stronger because of the antibacterial properties of breast milk.
Rarely, you might find nursing on the affected breast too painful. If that’s the case, one option is to allow the milk to flow out from the affected breast onto an absorbent cloth or towel while you have your baby nurse on the other breast. After relieving some of the pressure, you might be able to finish nursing on the affected breast without too much discomfort. Another option is to pump the breast and then either store the milk or feed it to your baby.
The discomfort of mastitis can be discouraging, but treatment can quickly help clear up the problem, allowing you to continue to enjoy the great benefits of breastfeeding.
How to Prevent Mastitis
Here are some ways to try to prevent mastitis in the first place:
- Switch up your breastfeeding positions to fully empty each breast.
- Make sure your baby is properly latched on to your breast.
- Feed your baby for as long as she will eat.
- Don't leave too much time between feedings. For example, if you usually feed your baby about every two hours, try to stick to that schedule.
- Apply a warm, wet washcloth to your breasts or take a warm shower before breastfeeding, as this can help get the milk flowing freely — even if you don't have mastitis.
Eventually, when you decide it's time to stop breastfeeding and wean your baby, you may wonder how to dry up your milk supply without getting mastitis. The key is to wean gradually. Ask your lactation consultant or healthcare provider for guidance.
FREQUENTLY ASKED QUESTIONS
- Can you breastfeed with mastitis?
Yes. In fact, continuing to breastfeed will help clear the infection. Your breast milk also helps keep your baby’s immune system strong.
- How can I treat mastitis at home?
- Drink lots of fluids
- Rest
- Empty the breast at each feeding
- Keep your regular feeding times
- Apply a warm compress to the breast
- Gently massage the warmed breast just before and during feeds
- Go braless and wear loose-fitting tops
- What are the first signs of mastitis?
- A tender, hard lump in one of your breasts
- Feeling achy and fatigued
- Fever
- Red patches on your breast
- What can happen if mastitis is left untreated?
If left untreated, symptoms can worsen and an abscess could form within the affected breast. If an abscess forms, it may need to be drained surgically by your healthcare provider. Breastfeeding or pumping with mastitis can be difficult and frustrating. Try to be patient and gentle with yourself during this time. With good at-home care under the direction of your healthcare provider, it won't be long until you're able to get back to enjoying this bonding time with your baby. For a little extra encouragement, check out this video guide on breastfeeding your baby.
How we wrote this article The information in this article is based on the expert advice found in trusted medical and government sources, such as the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. You can find a full list of sources used for this article below. The content on this page should not replace professional medical advice. Always consult medical professionals for full diagnosis and treatment.




